Probiotic - before or after an antibiotic? What really matters
See the key rules for taking a probiotic while on antibiotic therapy.


Learn more about our editorial process
.

Learn more about our editorial process
.

Learn more about our editorial process
.

Learn more about our editorial process
.
Why you can trust us
Articles on Natu.Care are written based on scientific research, data from government websites and other reliable sources. The texts are written in cooperation with doctors, nutritionists and other health and beauty experts. Articles are reviewed before publication and during significant updates.
.Learn more about our editorial process
.Information about advertisements
Content on Natu.Care may contain links to products from the sale of which we may receive a commission. When creating content, we adhere to high editorial standards and take care to be objective about the products discussed. The presence of affiliate links is not dictated by our partners, and we select the products we review ourselves completely independently.
.Learn more about our terms and Conditions
.A quarter of a century ago, doctors were still eagerly prescribing antibiotics for most colds, even "just in case you get infected". It is hardly surprising, as the patients themselves were asking for these wonderful pills.
And yet, it turned out that the antibiotics were not enough.
And yet it turned out that antibiotics are not so nice at all. They have a lot of side effects and can be... bombous to the gut microbiota (no, that's not good). Fortunately, the fad of shunning antibiotics is passing, and specialists are placing increasing importance on supplementing antibiotic therapy with probiotics.
Well, that's cool. At first glance, the matter seems simple: you sip probiotics for the antibiotic. But the longer you think about it... If the antibiotic kills the bacteria, won't it also kill the ones in the preparation? Yes, it can. That's why you're about to learn all about how to take a probiotic while on antibiotic therapy.
.
From this article you will learn:
- Whether you can swallow an antibiotic and a probiotic together. .
- How to take probiotics to squeeze the most good out of them.
- How to take probiotics.
- Why take probiotics while on antibiotics.
- Why take probiotics while on antibiotics.

Odkryj korzyści, jakie niesie ze sobą Maślan Sodu Premium od Natu.Care!
Natu.Care Maślan Sodu Premium
Poznaj Maślan Sodu Premium – najwyższej jakości suplement wspierający zdrowie jelit. Maślan sodu pomaga w regeneracji nabłonka jelitowego, poprawia trawienie i wspiera naturalną równowagę mikroflory.
Sprawdź cenę
W końcu się lepiej czuję! Pożegnałam się ze wzdęciami i zaparciami a do tego poprawił się stan mojej cery bo zdrowe jelita to też zdrowa i piękna skóra. Polecam!@Klaudia F.
See also:
.
- All about probiotics
- When to take probiotics
- When probiotics do harm
- Gynecological probiotics
- Probiotics for the gut
- Probiotics for irritable bowel
- Probiotic for pregnant women
Whether to take a probiotic before or after an antibiotic?
.
Whether you take a probiotic before or after an antibiotic is a secondary issue. The most important thing is to keep an appropriate interval between the drug and the probiotic capsules (shield). It is best to take the probiotic 2-3 hours before or after the antibiotic. Use it from the first day of antibiotic treatment and about 1-2 weeks afterwards.
During antibiotic treatment, it is a good idea to remember to take a shielding formula containing beneficial bacteria at the same time. It is recommended to start taking probiotics from the first day of antibiotic therapy. It is advisable to continue taking them even two weeks after the end of treatment, in order to allow the intestinal flora to fully regenerateand.
There is no clear answer to the question of whether probiotics should be taken before or after an antibiotic. Choosing the right time depends on the specific preparation. Some should be taken on an empty stomach, for example half an hour before breakfast and at least 2 hours before the first antibiotic dose of the day. Others are recommended to be taken 2-3 hours after the antibiotic.
Whatever scheme you choose, do not take a probiotic at the same time as an antibiotic. The antibiotic can destroy most of the probiotic bacteria before they can reach the gut and begin to populate it.
It is possible to take a probiotic at the same time as an antibiotic.
However, there are some probiotic strains that are resistant to antibiotics. An example is yeast Saccharomyces boulardii, which is the gold standard for the treatment of antibiotic-induced diarrhoea. They are certainly worth looking for in the formulation of shielding probiotic preparts.
The most important principles of probiotic use
.
Here are 7 rules to implement when using a probiotic for antibiotic therapy.
It is important to look for these rules.
1. Choose good strains. Before buying a prebiotic product, make sure that the strains of bacteria it contains are not sensitive to the antibiotic in question. It is best to consult with your pharmacist or doctor about your choice.
.
2. Check the composition. Good quality formulations should contain a three-part designation of the names of the probiotic bacteria, with an indication of the specific strain most often denoted by a numerical-letter code. Also look for information on CFU, or colony-forming unit, which translates as 'colony-forming units'. CFUs show how many bacteria one dose of a probiotic contains.
3. Read the leaflet. It is in it (or on the packaging) that you will find information on how to store the product (some require keeping it in the fridge, others at room temperature) and directions on how to take it. There are two main schools for taking probiotics: in the morning on an empty stomach -there is less acid in an empty stomach, which increases the survival of probiotic bacteria on their way to the gut; in the evening just before bed -when the gut is working more slowly and it is easier for bacteria to colonise. Which strategy to choose depends on the strains of bacteria a particular probiotic contains.
According to the principles of chronopharmacology, the peak of intestinal function occurs between 12-13pm, however, perhaps this morning is a better idea..
 .
.
Ilona Krzak Master of Pharmacy
.
4. Comply with the dosage. Take the probiotic in the daily dose recommended to you by your doctor, pharmacist or the manufacturer of the respective preparation. Do not increase this dose on your own - an excess of probiotics can also harm you.
.
5. Maintain a time buffer. Take your probiotic dose 2-3 hours apart from your antibiotic tablet. Although some strains of bacteria are resistant to antibiotics, this action will certainly not harm you. And it's better to blow off steam.
.
6. Don't sip hot. Aside from the fact that hot drinks and food, according to the WHO, can increase the risk of oral and gastrointestinal cancers, sipping probiotics with hot coffee or tea can... boil them. Dead ones, unfortunately, are of no use to you.
.
7. Avoid alcohol. Consuming alcoholic beverages with certain types of antibiotics can seriously endanger your health (and sometimes your life). But even if you have finished taking an antibiotic but are still continuing probiotic therapy, alcohol is still not recommended. This is because it can deplete the gut flora and your probiotic treatment fails.
I have also come across a statement about using vitamin C with a probiotic at the same time, as it has an antioxidant effect and protects the bacteria from damage..
 .
.
Ilona Krzak Master of Pharmacy
.
Why do you need a probiotic when on antibiotics?
.
Imagine that your gut is like a city. When you get sick, it is invaded by an alien army of brutal colonisers who want to take over all the buildings. An antibiotic is... well, like a nuclear bomb. It effectively gets rid of the enemies, but it also does a purge among the inhabitants - survivors are scarce.
For your city to function, it needs its tenants. Without them, buildings will fall into disrepair, transport won't function, shops will be closed and so on. That's what you take probiotics for - so that your little, bacterial town can keep going.
Antibiotics are powerful tools in the fight against bacteria that cause disease. They are capable of eradicating these harmful micro-organisms or at least inhibiting their growth.
Antibiotics are a powerful tool in the fight against disease.
Nevertheless, antibiotics are not perfect. Their action is not selective, meaning that they cannot distinguish between harmful bacteria and those that are beneficial to you and necessary for the body to function properlyand.
The consequence of antibiotic therapy is often the destruction of the friendly gut flora. This phenomenon can lead to all sorts of gastrointestinal problems. The most common of these are diarrhoea and heartburnand.
The use of antibiotics and the degradation of the gut flora can also affect our mental condition..
 .
.
Ilona Krzak Master of Pharmacy
.
One way to protect and restore this valuable bacterial flora is to use probiotics during antibiotic therapy. Probiotics are live cultures of bacteria that are beneficial to your health.
Probiotic bacteria residing in your gut affectand:
- enhancing digestive processes (the stomach says "thank you"), .
- more efficient absorption of nutrients from food (you absorb more vitamins and minerals), .
- protecting the gut and preventing toxins and pathogens from entering the bloodstream (liver breathes a sigh of relief),
- stimulation of immune system cells (you have better immunity), .
- production of hormones and neurotransmitters that affect brain function (you have greater resistance to stress and a better mood), .
- health of the genitourinary system and prevention of its infections (less bladder inflammation and intimate infections).
Probiotic bacteria produce certain vitamins. In addition, it has been proven that Lactobacillus plantarum v299 increases the absorption of iron from food.
 .
.
Ilona Krzak Master of Pharmacy
.
Additionally, probiotics form a shield in the gut that protects you from pathogenic microbes. Probiotic bacteria make it difficult for pathogens to adhere to the intestinal walls, take away their nourishment, and produce substances that destroy these dangerous microorganismsand.
Taking probiotics can help restore friendly bacteria that have been destroyed by antibiotics, helping to protect the gastrointestinal tract from the unpleasant side effects of antibiotic therapy.
Best products for gut health:
Premium Sodium Butyrate
Product description
Premium Sodium Butyrate is a natural support for your digestive system. With a high dose of butyric acid (940 mg), it supports the regeneration of the intestinal mucosa, improving gut health and function, and aids in the absorption of nutrients. By taking care of your intestines, you're taking care of the health of your entire body.
Studies involving people suffering from irritable bowel syndrome confirm that sodium butyrate is ideal for supporting issues related to bacterial flora imbalances (for example, after antibiotic therapy), constipation and diarrhea, inflammation of the intestinal mucosa, or a diet low in fiber.
Premium Sodium Butyrate capsules are made using the innovative DRcaps® technology. This guarantees that the active ingredients in the product are protected from the destructive effects of stomach acids and digestive enzymes. As a result, we can be sure that the beneficial ingredients are released in the small intestine and are fully absorbed by our body.
Premium Sodium Butyrate from Natu Care is 100% tested, and its composition contains only the highest quality raw materials.
Pros and cons
Pros:
- Supports digestive system function
- Helpful for various gastrointestinal conditions, including IBS
- High dose of butyric acid in each capsule
- Eco-friendly, clean, and tested composition
- Free from added sugar, gluten, GMOs, and lactose
- Innovative capsule technology - DRcaps
Cons:
- None
Additional Information
Take 3 capsules daily at any time of the day, preferably with a meal. Swallow the capsules whole with water.
Premium Sodium Butyrate is intended for adults.
The product should be used under medical supervision.
User review
I've been using the product for 2 weeks. My stomach feels lighter, and my digestion has improved. I recommend it.
Sundose° Daily Lightness°
Product description
Sundose° Daily Lightness° is a formula thatós supports the stomach and liver, reduces the frequency of gasóing and bloating, and supports optimal digestion. The formula contains no unnecessary additivesós, and the composition of the active ingredients (e.g. curcumin with piperine) mutually enhances their absorption.
The dietary supplement from Sundose comes in two flavour versions: orange and green.
Pros and cons
Sundose° Daily Lightness° is a formula thatós supports the stomach and liver, reduces the frequency of gasóing and bloating, and supports optimal digestion. The formula contains no unnecessary additivesós, and the composition of the active ingredients (e.g. curcumin with piperine) mutually enhances their absorption.
The dietary supplement from Sundose comes in two flavour versions: orange and green.
Additional information
Sundose° Daily Lightness° is a formula thatós supports the stomach and liver, reduces the frequency of gasóing and bloating, and supports optimal digestion. The formula contains no unnecessary additivesós, and the composition of the active ingredients (e.g. curcumin with piperine) mutually enhances their absorption.
The dietary supplement from Sundose comes in two flavour versions: orange and green.
Sundose° Daily Lightness° is a formula thatós supports the stomach and liver, reduces the frequency of gasóing and bloating, and supports optimal digestion. The formula contains no unnecessary additivesós, and the composition of the active ingredients (e.g. curcumin with piperine) mutually enhances their absorption.
The dietary supplement from Sundose comes in two flavour versions: orange and green.
Asecurin IB
Product description
Asecurin IB is a synbiotic, i.e. a combination of a probiotic and a prebiotic. It contains bacteria and yeast to support the intestines and digestive system, as well as inulin, whichós food for these microorganisms. The addition of a prebiotic supports and accelerates the growth of beneficial bacterial flora in the intestines.
Pros and cons
Asecurin IB is a synbiotic, i.e. a combination of a probiotic and a prebiotic. It contains bacteria and yeast to support the intestines and digestive system, as well as inulin, whichós food for these microorganisms. The addition of a prebiotic supports and accelerates the growth of beneficial bacterial flora in the intestines.
Additional information
Asecurin IB is a synbiotic, i.e. a combination of a probiotic and a prebiotic. It contains bacteria and yeast to support the intestines and digestive system, as well as inulin, whichós food for these microorganisms. The addition of a prebiotic supports and accelerates the growth of beneficial bacterial flora in the intestines.
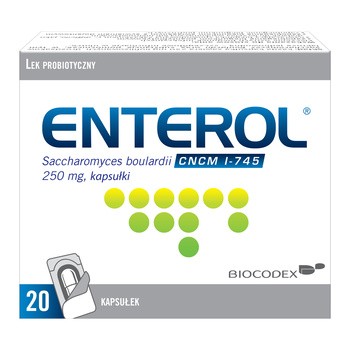
Biocodex Enterol
Product description
Enterol is an OTC medicine containing a strain of yeastów particularlyóhelpful in the treatment of diarrhoea caused by infections or so-called travel diarrhoea. It is also recommended as a protective treatment of the intestines during antibiotic intake.
.
Pros and cons
Enterol is an OTC medicine containing a strain of yeastów particularlyóhelpful in the treatment of diarrhoea caused by infections or so-called travel diarrhoea. It is also recommended as a protective treatment of the intestines during antibiotic intake.
.
Additional information
Enterol is an OTC medicine containing a strain of yeastów particularlyóhelpful in the treatment of diarrhoea caused by infections or so-called travel diarrhoea. It is also recommended as a protective treatment of the intestines during antibiotic intake.
.
Enterol is an OTC medicine containing a strain of yeastów particularlyóhelpful in the treatment of diarrhoea caused by infections or so-called travel diarrhoea. It is also recommended as a protective treatment of the intestines during antibiotic intake.
.
Product description
Using Panaseus Digestive Formula can help improve intestinal health by supporting the intestinal barrier, reducing inflammation, protecting against damage and restoring healthy intestinal microflora.
Experience a rós difference in gut function with plant extracts, amino acids and probiotic bacteria.
Pros and cons
Using Panaseus Digestive Formula can help improve intestinal health by supporting the intestinal barrier, reducing inflammation, protecting against damage and restoring healthy intestinal microflora.
Experience a rós difference in gut function with plant extracts, amino acids and probiotic bacteria.
Additional information
Using Panaseus Digestive Formula can help improve intestinal health by supporting the intestinal barrier, reducing inflammation, protecting against damage and restoring healthy intestinal microflora.
Experience a rós difference in gut function with plant extracts, amino acids and probiotic bacteria.
Does every antibiotic require a probiotic cover?
.
No, not every antibiotic requires probiotic therapy. It depends on the spectrum of action of the preparation, i.e. how many types of bacteria the substance it contains acts on. Most so-called 'first-line' antibiotics, i.e. those prescribed by the doctor in the first instance, have a very broad spectrum of action: they destroy most bacteria - both the 'good' and the 'bad' ones. Why is this so?"
To find out which specific strain of bacteria is responsible for the illness you have seen your doctor with would require specialised tests. With most diseases, it is a waste of time to do so.
The
To see what kind of bacteria you are dealing with, a culture with antibiograms is done and it is checked which antibiotics the strain grown is sensitive to. This is when targeted therapy can be put in place, limiting side effects. However, sometimes it takes a very long time to grow a colony of bacteria. The patient cannot therefore be left untreated..
 .
.
Ilona Krzak Master of Pharmacy
.
Additionally, some of the pathogenic microbes are structured so similarly to beneficial bacteria that scientists have so far failed to isolate a substance that would selectively destroy them, leaving the rest of the bacterial flora alone.
There are, however, a number of other microbes that have been found to be very similar to beneficial bacteria.
There are, however, narrow-spectrum antibiotics. Returning to the analogy of a city under siege, these drugs are like snipers. They target the enemy invaders precisely, without doing much harm to the inhabitants.
And what if you don't know what to do?
What if you don't know that you are taking a sniper and not a nuclear bomb and... you are going to take probiotics anyway? If you take probiotic preparations for 2-4 weeks and do not exceed the manufacturer's recommended doses, you are completely fine. Probiotics can also be used prophylacticallyand.

Sprawdź, za co pokochały go tysiące klientek Natu.Care Premium Omega-3ᵀᴳ -15% z kodem BLOG15
Natu.Care Omega-3ᵀᴳ Premium
Natu.Care Omega-3ᵀᴳ Premium dla zdrowia serca, mózgu i odporności. Najlepsza przyswajalność. Optymalna dawka 750 mg. Przebadana przez niezależne laboratorium.
Zobacz więcej
Produkt ma super skład, transparentną etykietę i co dla mnie jest ważne – małe kapsułki do połknięcia. Nie ma też nieprzyjemnego efektu odbijania rybą, który miałam spożywając inne produkty. Widzę znaczną poprawę odporności. Polecam!@Kasia P.
See also:
.
Summary
.
- Probiotics while on antibiotic therapy help to restore the gut microbiota that may be depleted by the drug.
- Probiotics can help to restore the gut microbiota.
- Take probiotics throughout the period you are on the antibiotic and continue for about two more weeks, after you have finished treatment with the drug.
- Probiotics can be used to help restore the gut microbiota that may be depleted by the drug.
- You can take the probiotic both on an empty stomach - before the first dose of the antibiotic, and in the evening - after taking the last dose of the medication. .
- It is most important to maintain a time interval between the times you take the antibiotic and the probiotic - this should be at least 2 hours. .
- During probiotic treatment, refrain from drinking alcohol and do not sip probiotic preparations with hot drinks. .
- Probiotics will help to rebuild the bacteria living in your intestines that may have been destroyed by the antibiotic. This will protect you from gastrointestinal complaints and a decrease in immunity. .
FAQ
.Do probiotics need to be taken with food?
.No, probiotics do not need to be taken with food. However, it is important to take them regularly. If you choose a probiotic in capsule form, simply sip it with plenty of water. Some preparations may also be more effective if taken before a meal.
.Why? Because the stomach will then contain less acid, allowing more probiotic bacteria to survive and reach the gut. However, always follow the manufacturer's instructions on how to take the probiotic.
Do not take the probiotic at any time.
Do probiotics need to be kept in the fridge?
.Some probiotics need to be kept in the fridge, but this does not apply to all preparations. To store probiotic properly and retain its properties, check the manufacturer's recommendations for storage.
Outside of the correct temperature, most preparations should be kept in a shaded and dry place.
Is it possible to take a probiotic before bedtime?
.It is possible to take probiotics before bedtime. At night, the intestines and digestive system slow down, making it easier for bacteria to colonise. Take probiotic at the earliest two hours after your last antibiotic dose.
What is the best way to sip a probiotic?
Probiotic is best sipped with water. Avoid milk, grapefruit juice, coffee or tea as they can interfere with the bacteria. Water is neutral and does not affect the ingredients in the formula. For example, the acid in grapefruit juice can destroy the probiotic bacteria before they reach the intestines.
What happens when you take an antibiotic without a cover?
.Taking an antibiotic without a cover can lead to disruption of the gut microflora. By eliminating pathogenic bacteria, antibiotics also destroy the beneficial bacteria in the gut. The result can be diarrhoea, bloating and even the development of pathogenic flora such as Clostridium difficile.
To prevent this, take probiotics to help rebalance the microflora. Take them a minimum of 2 hours before or after an antibiotic so that they are not destroyed by it.
Additionally, ensure a diet is rich in fibre. Fruit, vegetables or whole-grain bread will help to regenerate the intestinal flora, providing a food source for probiotic bacteria.
Is it possible to take a probiotic on an empty stomach?
.Yes, probiotics can be taken on an empty stomach as they do not irritate the stomach. Taking probiotics before a meal can also increase the survival rate of certain strains that are sensitive to digestive juices. When the stomach is empty, the amount of acid it contains is less and more bacteria will be able to pass into the gut.
Does a probiotic stimulate appetite?
.Probiotics are not directly related to appetite stimulation. Their main role is to improve gut health, which can indirectly affect appetite, but this is not their primary action. Probiotics help with proper digestion, which can lead to better utilisation of nutrients from food.
Consult a dietitian if you have appetite problems. He or she may recommend changes to your diet, such as introducing more calorie-dense foods or more frequent but smaller meals.
Sources
.See all
.Becattini, S., Taur, Y., & Pamer, E. G. (2016). Antibiotic-Induced Changes in the Intestinal Microbiota and Disease. Trends in Molecular Medicine, 22(6), 458-478. https://doi.org/10.1016/j.molmed.2016.04.003
Han, S., Lu, Y., Xie, J., Fei, Y., Zheng, G., Wang, Z., Liu, J., Lv, L., Ling, Z., Berglund, B., Yao, M., & Li, L. (2021). Probiotic Gastrointestinal Transit and Colonization After Oral Administration: A Long Journey. Frontiers in Cellular and Infection Microbiology, 11. https://www.frontiersin.org/articles/10.3389/fcimb.2021.609722
Jakobsson, H. E., Jernberg, C., Andersson, A. F., Sjölund-Karlsson, M., Jansson, J. K., & Engstrand, L. (2010). Short-Term Antibiotic Treatment Has Differing Long-Term Impacts on the Human Throat and Gut Microbiome. PLOS ONE, 5(3), e9836. https://doi.org/10.1371/journal.pone.0009836
Judkins, T. C., Archer, D. L., Kramer, D. C., & Solch, R. J. (2020). Probiotics, Nutrition, and the Small Intestine. Current Gastroenterology Reports, 22(1), 2. https://doi.org/10.1007/s11894-019-0740-3
Rashid, M.-U., Zaura, E., Buijs, M. J., Keijser, B. J. F., Crielaard, W., Nord, C. E., & Weintraub, A. (2015). Determining the Long-term Effect of Antibiotic Administration on the Human Normal Intestinal Microbiota Using Culture and Pyrosequencing Methods. Clinical Infectious Diseases, 60(suppl_2), S77-S84. https://doi.org/10.1093/cid/civ137
Sanders, M. E., Guarner, F., Guerrant, R., Holt, P. R., Quigley, E. M., Sartor, R. B., Sherman, P. M., & Mayer, E. A. (2013). An update on the use and investigation of probiotics in health and disease. Gut, 62(5), 787-796. https://doi.org/10.1136/gutjnl-2012-302504
Shahrokhi, M., & Nagalli, S. (2023). Probiotics. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK553134/
Stewardson, A. J., Gaïa, N., François, P., Malhotra-Kumar, S., Delémont, C., Tejada, B. M. de, Schrenzel, J., Harbarth, S., & Lazarevic, V. (2015). Collateral damage from oral ciprofloxacin versus nitrofurantoin in outpatients with urinary tract infections: A culture-free analysis of gut microbiota. Clinical Microbiology and Infection, 21(4), 344.e1-344.e11. https://doi.org/10.1016/j.cmi.2014.11.016
Tegegne, B. A., & Kebede, B. (2022). Probiotics, their prophylactic and therapeutic applications in human health development: A review of the literature. Heliyon, 8(6), e09725. https://doi.org/10.1016/j.heliyon.2022.e09725
.Zaura, E., Brandt, B. W., Teixeira de Mattos, M. J., Buijs, M. J., Caspers, M. P. M., Rashid, M.-U., Weintraub, A., Nord, C. E., Savell, A., Hu, Y., Coates, A. R., Hubank, M., Spratt, D. A., Wilson, M., Keijser, B. J. F., & Crielaard, W. (2015). Same Exposure but Two Radically Different Responses to Antibiotics: Resilience of the Salivary Microbiome versus Long-Term Microbial Shifts in Feces. mBio, 6(6), 10.1128/mbio.01693-15. https://doi.org/10.1128/mbio.01693-15
.
Editorials
Meet the team

Ilona Krzak obtained her Master of Pharmacy degree from the Medical University of Wrocław. She did her internship in a hospital pharmacy and in the pharmaceutical industry. She is currently working in the profession and also runs an educational profile on Instagram: @pani_z_apteki


Chondroitin helps the joints and other elements of the body.

Glutathione is one of the most potent antioxidants for supporting the body's health. Find out how it works and where to get it from.

See why hip joints hurt and how to treat their ailments.